Abstract
Background: Painful vaso-occlusive crises (VOC) are a frequent and debilitating complication of sickle cell disease (SCD). The exact mechanism of transition from steady state to VOC is not well understood although it is thought to occur due to progressive blockage of the microvasculature with rigid sickle shaped red blood cells. Thus, any trigger that decreases the microvascular blood flow increases the red blood cell transit time and can promote entrapment of sickled cells in the microvasculature and progression to VOC. Environmental factors such as exposure to cold wind and changes in weather are common triggers of VOC and have been shown to be associated with increased frequency of hospitalizations for pain in patients with SCD. There is limited experimental data in literature on the physiologic effects of these factors on peripheral perfusion in SCD.
Objective: To study the effect of graded thermal stimuli on the peripheral microvascular blood flow in SCD.
Methods: 17 SCD and 11 control (healthy or sickle trait) subjects aging 13 to 39 years were exposed to graded thermal stimuli via TSA- II Neurosensory analyzer thermode that was placed on the thenar eminence. Individual threshold temperatures for heat and cold detection, heat and cold pain were applied and changes in the microvascular blood flow were measured on the contralateral thumb using photo-plethysmography (PPG).
The vasoconstriction response within the complex microvascular blood flow signal was detected using cross-correlation technique. In order to quantify the vasoconstriction response, we calculated mean blood flow (MBF) from the PPG amplitude during each of these stimuli and compared to the MBF at baseline.
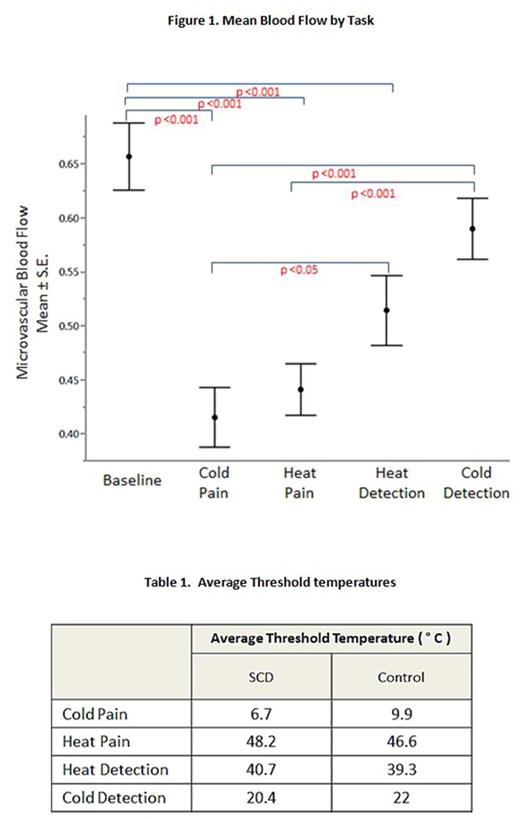
Results: Cross correlation analysis showed that cold pain caused significant vasoconstriction response in 75% of the subjects, followed by heat pain (57%), cold detection (39%) and heat detection (18%).There was a significant drop in the MBF during cold pain, heat pain and heat detection when compared to baseline MBF (p <0.001) where cold pain caused the greatest drop in MBF (Figure 1). SCD subjects trended towards greater percent change in MBF from baseline across all the threshold temperatures but there was no significant difference between the two groups. The average threshold temperatures were comparable across the two groups with no significant differences in thermal sensitivity detected between SCD and controls (Table 1).
Conclusions: Exposure to graded thermal stimuli causes a progressive drop in microvascular blood flow with exposure to cold pain eliciting the strongest vasoconstriction response. The vasoconstriction occurred in the contralateral hand at an average of 10 seconds after the stimulus, suggesting a neurally mediated mechanism. Although there was no significant difference in vasoconstriction responses between SCD and controls, the drop in microvascular blood flow in sickle cell patients can increase the likelihood of entrapment of the sickled red blood cells in the microvasculature leading to vaso-occlusion. These findings are consistent with extensive reports in literature that exposure to extremes of cold weather is associated with a higher frequency of VOC. This suggests that neurally mediated decrease in the microvascular blood flow is likely an important factor in the pathophysiology behind cold exposure leading to VOC in SCD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal